In a 2012 report, Accelerating Progress in Obesity Prevention(APOP), the National Academy of Medicine recommended five areas of focus to address obesity in the United States:
- Make physical activity a routine part of life
- Improve food and beverage environments
- Transform the content/delivery of messages around physical activity and nutrition
- Expand the role of healthcare providers, insurers, and employers
- Make schools a national focal point
While the APOP report offers useful guidance in developing obesity interventions for the general public, it does not directly address the limited efficacy of such interventions in socially and economically disadvantaged communities. Dissemination of one-size-fits-all approaches that do not address differences in community resources and social agency may have a paradoxical effect of increasing disparities in the prevalence of obesity and its related comorbidities. Between 1988 and 2008, some subpopulations experienced greater increases in obesity prevalence than others. Data from the National Health and Nutrition Examination Surveys indicate that the prevalence of obesity in adults is higher among non-Hispanic blacks (48.1%) and Hispanics (42.5%) than among non-Hispanic whites (34.5%) and non-Hispanic Asians (11.7%). Among white women, obesity prevalence increases as income and level of education decrease.
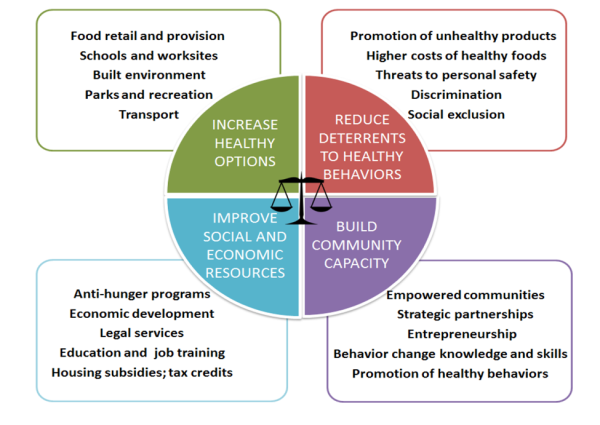
Dr. Shiriki Kumanyika’s recent perspective —“Getting to Equity in Obesity Prevention”— builds on the APOP recommendations and offers an operational, equity-oriented obesity prevention action framework wherein communities strategically implement interventions in ways that reduce, rather than exacerbate, health disparities.
While the core elements of this framework can be applied in any community, the design highlights particular pathways and intervention combinations that may work synergistically to mitigate inequities within and between populations. This framework goes beyond promotion of healthy eating and physical activity, indicating that substantial investment in upstream determinants of health such as social and economic resources is critical to addressing obesity. When bundled with anti-hunger programs like SNAP and WIC, improved employment opportunities, and non-discriminatory policies that improve housing conditions, traditional obesity prevention efforts are more likely to generate substantial, population-wide improvements in health.
The identification of unique community-level challenges and assets through collaborations of relevant stakeholders is critical for the development of sustainable, equitable solutions to obesity prevention and treatment. To date, most policy solutions have been directed at the left upper quadrant of the figure. Less work has focused on making less healthful products less available. Broader strategies that begin to address social determinants of obesity, build capacity, and empower communities represent a more comprehensive and sustainable approach to reduce the disparities associated with obesity. Dr. Kumanyika’s framework provides an innovative and welcome perspective that should serve as a starting point for those building comprehensive, cross-sector interventions to advance community health and promote equity in obesity prevention efforts.