Understanding Obesity
Understanding Obesity
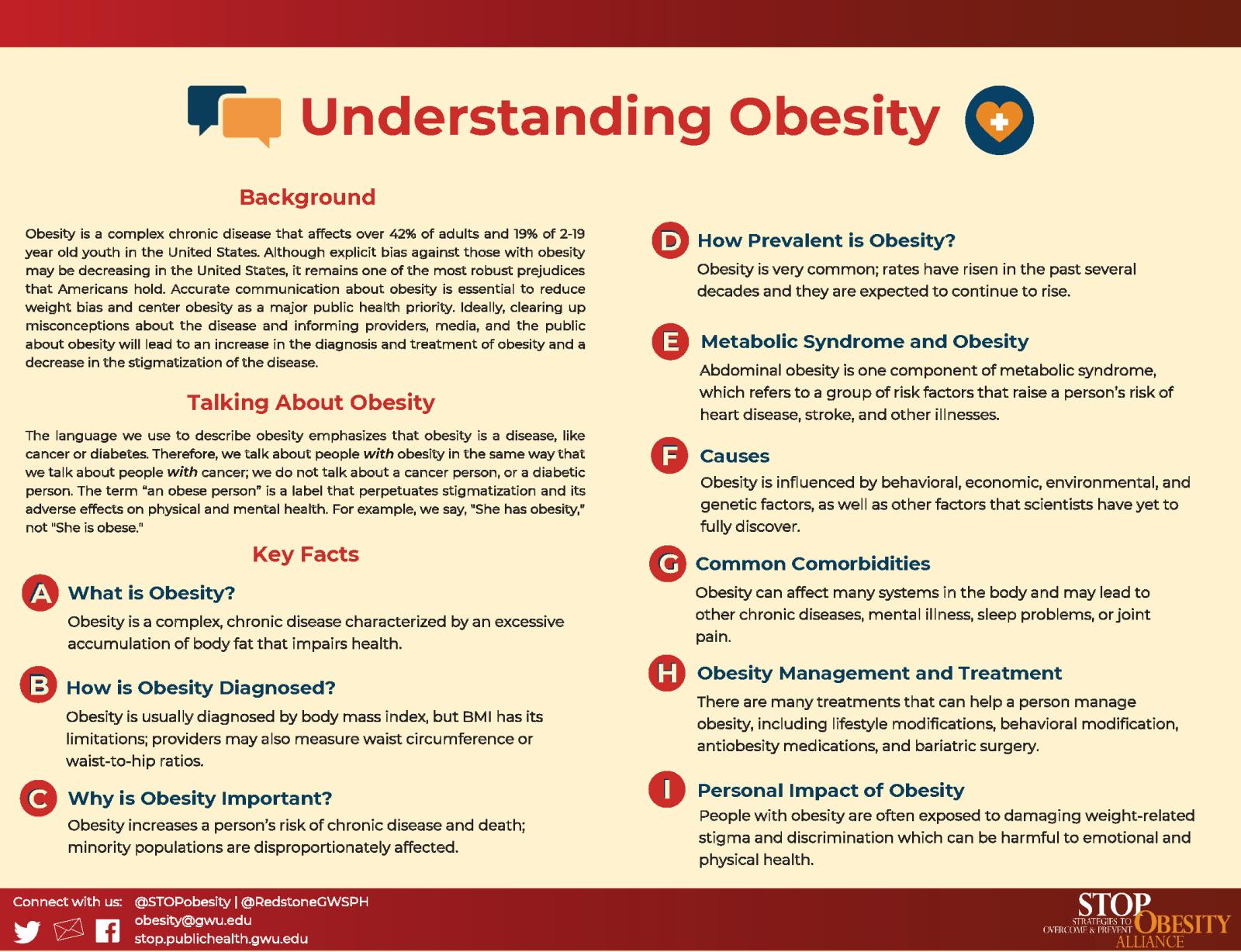
Although obesity is highly prevalent and widely known, misconceptions abound and can cause real harm to those living with the disease.
To address this misinformation, STOP created a messaging framework called Understanding Obesity, which features accessible and unbiased information about the harms of weight bias, as well as guidance on destigmatizing the language used to discuss obesity.
Understanding Obesity
Download: Understanding Obesity Messaging Framework (PDF)
I. Background
Obesity is a complex chronic disease that affects over 42% of adults and 19% of 2-19 year old youth in the United States.1,2 Obesity occurs when an excessive accumulation of body fat impairs health. The onset of obesity can occur in childhood, adolescence, or adulthood and is influenced by behavioral, economic, environmental, and genetic factors. Although safe and effective obesity treatments exist, they are underutilized by providers who often lack training in treating obesity.3 One significant challenge to the treatment of obesity is that this disease is often misunderstood and misrepresented; obesity is often portrayed as a matter of personal failing, rather than the consequence of complex individual and environmental interactions that it is.
Although explicit bias against those with obesity may be decreasing in the United States,4 it remains one of the most robust prejudices that Americans hold.5 Experiencing stigmatizing language from a provider can discourage patients with obesity from continuing care, making effective communication imperative.6 The media plays a large role in perpetuating weight stigma by portraying those with obesity in an unfavorable light. Both the content of news articles about obesity and the images that accompany them often rely on negative stereotypes and reinforce the narrative that obesity is a matter of personal responsibility, rather than a complex disease.7,8 Accurate communication about obesity is essential to reduce weight bias and center obesity as a major public health priority. Ideally, clearing up misconceptions about the disease and informing providers, media, and the public about obesity will lead to an increase in the diagnosis and treatment of obesity and a decrease in the stigmatization of the disease.
II. Talking About Obesity
The language we use to describe obesity emphasizes that obesity is a disease, like cancer or diabetes. Therefore, we talk about people with obesity in the same way that we talk about people with cancer; we do not talk about a cancer person, or a diabetic person. The term “an obese person” is a label that perpetuates stigmatization and its adverse effects on physical and mental health. For example, we say, "She has obesity," not "She is obese."
III. Key Facts
-
A - What is Obesity?
-
- Obesity is a complex, chronic disease that affects hundreds of millions of people worldwide.9
- Obesity occurs when an excessive accumulation of body fat impairs health and is considered a risk factor for diseases like type 2 diabetes, heart disease, and some types of cancer.10
- A common calculation used to screen for obesity is body mass index (BMI), which is calculated by dividing a person’s weight in kilograms by their height in meters squared. Obesity is diagnosed at a BMI of 30, and a BMI of over 40 constitutes severe obesity.
- Obesity is a treatable medical condition that can be managed for better health with the help of a healthcare provider. This can take the form of weight loss, weight maintenance, or symptom management
-
B - How is Obesity Diagnosed?
-
- Using BMI to diagnose obesity has its limitations, because BMI only describes weight and height, not body composition.11
- Other methods of assessing obesity include waist-to-hip ratios and waist circumference. These measures can be used to determine abdominal fat, which increases the risk of several weight-related diseases.11
- Methods for determining body fat content are available but are not yet inexpensive, practical, accurate or accessible enough to be used in most practices.11
- Although accurately diagnosing obesity can be complex, it can be essential to getting appropriate treatment for many patients with obesity. Patients with a BMI ≥ 30 who receive a diagnosis of obesity are more likely to lose weight than patients with a BMI ≥ 30 who do not receive a diagnosis.12
-
C - Why is Obesity Important?
-
- Obesity has become a pandemic, interacting with undernutrition and climate change to create a global syndemic of poor health.13
- Obesity increases a person’s risk of chronic disease and death, as well as putting them at higher risk of severe illness from infectious diseases like COVID-19.10,14
- Obesity disproportionately affects already vulnerable populations including individuals with food insecurity, those with mental illnesses, and some racial and ethnic minority groups.14,15,16
- Obesity and obesity-related complications pose a significant financial burden to individuals and society through the medical costs, lost productivity, and disability claims.17
-
D - How Prevalent is Obesity?
-
- Obesity is very common; 42.4% of American adults had obesity in 2017-2018. Severe obesity is also becoming more common with a national rate of 9.2%.1
- Obesity rates have increased steadily over the past few decades and are expected to continue to climb. Projections suggest that the U.S. adult obesity rate in 2030 will be around 1 in 2, with severe obesity rates reaching nearly 1 in 4.18,19
- Obesity is much more common within some groups than others. Black women and Hispanic men and women all have obesity rates that are higher than the national average.1
- Although it is estimated that a majority of Americans have experienced obesity at some point in their lives,20 weight stigma remains prevalent and obesity remains underdiagnosed and undertreated.3,5,12
-
E - Metabolic Syndrome and Obesity
-
- Metabolic syndrome refers to a group of risk factors that raise a person’s risk of heart disease, stroke, and other illnesses.21
- Abdominal obesity is one component of metabolic syndrome. Other components of metabolic syndrome like high blood pressure and high blood sugar may also be related to obesity.21
- Not all people with obesity have metabolic syndrome. Some people with obesity are considered metabolically healthy and do not experience unhealthy insulin sensitivity or poor cardiovascular health.22
-
F - Causes
-
- Obesity is a complex disease influenced by behavioral, economic, environmental, and genetic factors. There are likely even more factors influencing obesity that scientists have yet to fully discover.23
- Food choices and physical activity both affect a person’s weight and health. The modern environment makes obesity more likely—ultra-processed foods high in calories are cheap and prevalent, and opportunities for physical activity are decreasing.23
- Differences in access can lead to health disparities; some Americans live in areas where healthy food is unaffordable and outdoor spaces are not safe enough for physical activity.24
- Obesity is highly heritable. Individuals with a genetic predisposition to obesity may be more susceptible to environmental factors.25
-
G - Common Comorbidities
-
- Obesity is related to many other chronic diseases including type 2 diabetes, osteoarthritis, heart disease, and cancer.10
- Obesity can affect many systems in the body and may lead to organ complications, such as non-alcoholic fatty liver disease and gallbladder disease.26
- Obesity and mental illnesses commonly co-occur, in part because weight gain is a side effect of many psychiatric medications.10,27
- Obesity is commonly accompanied by respiratory problems like sleep apnea, and chronic back or joint pain.26
-
H - Obesity Management and Treatment
-
- Many people with obesity manage their obesity through lifestyle modifications such as eating a nutritious diet and getting the recommended amount of physical activity. A 5-10% weight loss can significantly improve health for those with obesity.28
- For those with a BMI ≥ 30 or a BMI ≥ 27 with weight-related comorbidities, healthcare providers may prescribe anti-obesity medications. There are several FDA-approved medications for the treatment of obesity, and they are often paired with lifestyle modifications.29
- For those with a BMI ≥ 40 or a BMI ≥ 35 with weight-related comorbidities, healthcare providers may recommend bariatric surgery. There are several available bariatric surgery procedures. Eligibility for these procedures depends on a patient’s medical history and their health plan.30
-
I - The Personal Impact of Obesity
-
- People with obesity are often exposed to damaging weight-related stigma and discrimination, which can come from healthcare providers, family, friends, and the media. Prevalence estimates suggest that 19-40% of adults with obesity experience weight discrimination.31
- People with obesity may face stigma and unfair treatment in the workplace, ranging from inequitable hiring practices to unfair job termination.32
- Experiencing and internalizing weight stigma are harmful to emotional and physical health, negatively affecting both youth and adults.33,34
- Obesity can be associated with disability and impaired quality of life,35 though studies have shown that quality of life increases when people with obesity are able to access care such as bariatric surgery.36
IV. References
- Expand References
-
- Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief, no 360. Hyattsville, MD: National Center for Health Statistics. 2020
- Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. NCHS Health E-Stats. 2020
- Dietz WH, Baur LA, Hall K, et al. Management of obesity: Improvement of health-care training and systems for prevention and care. The Lancet. 2015;385(9986):2521-2533
- Kyle TK, Cready G, Thomas DM, Watts K, Nadglowski J. Indications That Explicit Bias about Obesity May Be Declining More in the U.S. Than in the U.K. Poster presented at: European and International Conference on Obesity (ECOICO2020); September 1-4, 2020; Virtual.
- Charlesworth TES, Banaji MR. Patterns of Implicit and Explicit Attitudes: I. Long-Term Change and Stability From 2007 to 2016. Psychological Science. 2019;30(2):174-192. doi:10.1177/0956797618813087
- Puhl R, Peterson JL, Luedicke J. Motivating or stigmatizing? Public perception of weight-related language used by health providers. Int J Obes. 2013; 37: 612-619.
- Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring). 2009;17(5):941-964. doi:10.1038/oby.2008.636
- Heuer CA, McClure KJ, Puhl RM. Obesity Stigma in Online News: A Visual Content Analysis. J Health Commun. 2011;16(9):976-987. doi: 10.1080/10810730.2011.561915
- World Health Organization. Obesity and Overweight. 2020. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- Centers for Disease Control and Prevention. Adult Obesity Causes & Consequences. https://www.cdc.gov/obesity/adult/causes.html. Published September 17, 2020. Accessed November 30, 2020.
- Lopez-Jimenez F, Miranda WR. Diagnosing obesity: beyond BMI. AMA Journal of Ethics. 2010;12(4):292-298.
- Ciemins EL, Joshi V, Cuddeback JK, Kushner RF, Horn DB, Garvey WT. Diagnosing Obesity as a First Step to Weight Loss: An Observational Study. Obesity. 2020;28(12):2305-2309. doi: https://doi.org/10.1002/oby.22954.
- Swinburn BA, Kraak VI, Allender S, et al. The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission report. The Lancet. 2019;393(10173):791-846. doi: 10.1016/S0140-6736(18)32822-8.
- Centers for Disease Control and Prevention. Overweight & Obesity. Obesity, Race/Ethnicity, and COVID-19.
https://www.cdc.gov/obesity/data/obesity-and-covid-19.html. Published January 8, 2021. - Pan L, Sherry B, Njai R, Blanck HM. Food insecurity is associated with obesity among US adults in 12 states. J Acad Nutr Diet. 2012;112(9):1403-1409. doi:10.1016/j.jand.2012.06.011
- Dickerson FB, Brown CH, Kreyenbuhl JA, et al. Obesity among individuals with serious mental illness. Acta Psychiatr Scand. 2006;113(4):306-313. doi:10.1111/j.1600-0447.2005.00637.x
- STOP Obesity Alliance. Costs of Obesity. 2020.
https://stop.publichealth.gwu.edu/files/Costs%20of%20Obesity.pdf - RWJF. National Obesity Monitor. The State of Childhood Obesity. https://stateofchildhoodobesity.org/monitor/.
- Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381(25):2440-2450.
- Stokes A, Ni Y, Preston SH. Prevalence and Trends in Lifetime Obesity in the U.S., 1988-2014. Am J Prev Med. 2017;53(5):567-575.
doi:10.1016/j.amepre.2017.06.008 - National Heart Lung and Blood Institute. Metabolic Syndrome. https://www.nhlbi.nih.gov/health-topics/metabolic-syndrome.
- Engin A. The Definition and Prevalence of Obesity and Metabolic Syndrome. Adv Exp Med Biol. 2017;960:1-17. doi:10.1007/978-3-319-48382-5_1
- STOP Obesity Alliance. Causes of Obesity. 2020. https://stop.publichealth.gwu.edu/fast-facts/causes-of-obesity
- Sallis JF, Floyd MF, Rodríguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125(5):729-737.
- Yang W, Kelly T, He J. Genetic epidemiology of obesity. Epidemiol Rev. 2007; 29: 49-61.
- Overweight and Obesity. National Heart Lung and Blood Institute. https://www.nhlbi.nih.gov/health-topics/overweight-and-obesity#:~:text=There%20are%20no%20specific%20symptoms,by%20measuring%20your%20waist%20circumference.
- Schwartz TL, Nihalani N, Jindal S, Virk S, Jones N. Psychiatric medication-induced obesity: a review. Obesity Reviews. 2004;5(2):115-121.
doi:https://doi.org/10.1111/j.1467-789X.2004.00139.x. - Ryan, D. H., & Yockey, S. R. Weight loss and improvement in comorbidity: differences at 5%, 10%, 15%, and over. Current Obesity Reports,
2017;6(2), 187-194. - Physician-supervised Weight-loss. Obesity Action Coalition. https://www.obesityaction.org/obesity-treatments/what-is-obesity-
treatment/physician-supervised-weight-loss/. - Bariatric Surgery and Devices. Obesity Action Coalition. https://www.obesityaction.org/obesity-treatments/what-is-obesity-
treatment/bariatric-surgery-and-devices/ - Spahlholz J, Baer N, König HH, Riedel-Heller SG, Luck-Sikorski C. Obesity and discrimination - a systematic review and meta-analysis of observational studies. Obes Rev. 2016;17(1):43-55. doi:10.1111/obr.12343
- Rudolph CW, Wells CL, Weller MD, Baltes BB. A meta-analysis of empirical studies of weight-based bias in the workplace. J Vocat Behav. 2009;74(1):1-10. doi: 10.1016/j.jvb.2008.09.008.
- Puhl RM, Himmelstein MS, Pearl RL. Weight stigma as a psychosocial contributor to obesity. Am Psychol. 2020;75(2):274-289. doi:
10.1037/amp0000538. - Alimoradi Z, Golboni F, Griffiths MD, Broström A, Lin CY, Pakpour AH. Weight-related stigma and psychological distress: A systematic review and meta-analysis. Clin Nutr. 2020;39(7):2001-2013. doi:10.1016/j.clnu.2019.10.016
- Ells LJ, Lang R, Shield JPH, et al. Obesity and disability – a short review. Obesity Reviews. 2006;7(4):341-345. doi: https://doi.org/10.1111/j.1467-789X.2006.00233.x.
- Kolotkin RL, Andersen JR. A systematic review of reviews: exploring the relationship between obesity, weight loss and health-related quality of life. Clin Obes. 2017;7(5):273-289. doi: https://doi.org/10.1111/cob.12203.