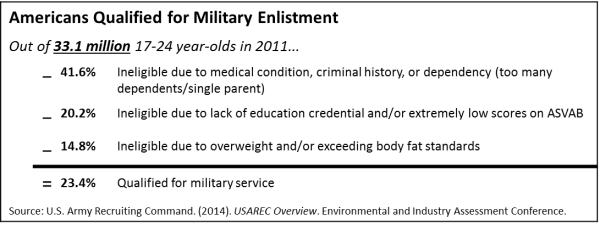
The national security of the United States depends on a fit military. Obesity in military personnel impairs fitness and affects both recruitment and retention. Along with poor academic performance and criminal behavior, nationwide increases in prevalence of overweight and obesity pose major challenges to U.S. military recruitment. Comparison of established military accession standard to population data from national health and behavior surveys (e.g. NHANES, BRFSS) reveals that fewer than 30% of the prime recruiting pool (17-24 year-olds not in college) meet the core military eligibility requirements. Being overweight prevents more than 10% of otherwise eligible recruits from service. Among actual applicants, failure to meet body composition standards increased 70% from 1995-2008 and is now the top medical disqualifier.
Based on self-reported weight and height, the prevalence of obesity among enlisted men and women rose from nearly 5% in 1995 to almost 13% in 2008. Analysis of recent health-records data released by the Pentagon indicated a similar trend, with clinical diagnoses of overweight jumping from 1.6% of military personnel in 2001 to 7.8% in 2015. Although each branch of service differs slightly in its body composition standards for enlistment and retention, Department of Defense (DoD) guidelines issued in 2002 mandate the upper limits for two common metrics: maximum BMI set between 25 and 27.5 kg/m2 and maximum allowable body fat set at or below 28% for men and 36% for women.
A 2008 survey of active-duty personnel found that 15% of men and 20% of women reported difficulty meeting weight and/or body fat standards. Failure to meet body-composition standards often results in ineligibility for promotion, frequent weigh-ins, and increased training intensity. The persistent focus on weight, and resulting weight bias, may partly account for the unusually high prevalence of disordered eating and unhealthy weight management strategies observed among military personnel and their families. In one recent study that surveyed service members with overweight and obesity, 49% of participants reported experiencing weight stigma. Perceived weight stigma was positively associated with maladaptive coping, depressive symptoms, and compensatory behaviors among participants. Each year, more than $60 million goes toward replacing the 1,200+ first-term enlistees discharged for excess weight.
The problem of obesity also affects military families and retirees. Data suggest that 30% of youth, 45% of military spouses, and 72% of veterans are either overweight or have obesity. Although broad military changes in dietary intake and sedentary behavior somewhat mirror those of the civilian population, the physical and psychosocial stress associated with stringent fitness standards, overseas deployments, and frequent relocations may put service members, their families, and veterans at increased risk for psychological and physiological changes that contribute to weight gain. TRICARE estimates that overweight and obesity cost the military health system nearly $106 million in lost productivity and $1.1 billion in associated medical expenditures annually.
Recognizing the need to bolster support for the physical and psychological health of U.S. soldiers, many military leaders and policymakers have begun to pilot innovative approaches to healthy weight management in the military community. Preventing Obesity in the Military Community is a newly established research program that targets obesity prevention and treatment during high-risk periods for weight gain—pregnancy and early infancy, adolescence, young adulthood (after the first tour of boot camp), and years immediately preceding/following departure from active duty. The Healthy Base Initiative (HBI)—a component of the Department of Defense’s "Operation Live Well" campaign—tested a series of short-term demonstration projects across 14 pilot sites to assess the ability of various environmental and behavioral interventions to make good nutrition, active lifestyles, and tobacco-free living the norm among service members and their families. Although the 1-2 year implementation period was too brief to capture meaningful population-level changes in prevalence of overweight and obesity, the HBI framework included an extensive family of performance measures that may be useful when assessing similar programs among civilian populations.
Left unaddressed, high rates of overweight and obesity among the military-age population pose a continual threat to national security. Within the military community, targeted investment in evidence-based programs that reduce weight stigma and promote healthy weight management across the lifespan are likely to improve personnel retention and readiness, reduce system-wide healthcare costs, and boost individual morale. These observations also emphasize that continued investments in programs and policies that improve nutrition and physical fitness to prevent obesity among young adults are essential to maintaining the pool of eligible recruits.