Although obesity imposes an enormous burden on our health care system and the economy, the present landscape of coverage for obesity care is piecemeal. Our fragmented healthcare system makes it difficult to know what care is available and how much it costs.
Without guidance on how to operationalize evidence-based obesity treatment modalities as health benefits, health care plans have taken vastly different approaches in determining what and how obesity treatment services are covered for their members. To complicate matters, information about what services are covered, for whom, and where and how care should be delivered, is spread across various administrative plan documents and sources.
As part of our efforts to improve the treatment and management of obesity, our team has been exploring which insurance carriers are paying for these services and if patients are utilizing treatment. In 2009 and 2017, we conducted a state-by-state analysis of Medicaid and State Employee Health Plan (SEHP) coverage for obesity prevention and treatment. The results of this research were published in Obesity.
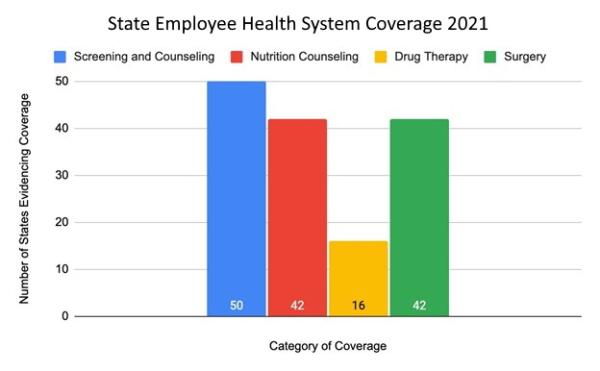
Last year, we collected new data on SEHP coverage of obesity benefits for plan year 2021. Our results are being published in the August edition of Obesity.
We reviewed publicly available documents, such as websites for state human resources departments, state pension boards, and health plans, to determine coverage for prevention and screening, nutrition counseling, drug therapy, and bariatric surgery. We found that all 50 states provided coverage for prevention and screening, 42 states provided coverage for nutrition counseling, 44 states covered bariatric surgery, but only 16 states provided coverage for pharmacotherapy treatment of obesity.
The new data collected in 2021 were compared to data collected in 2009 and 2017 to assess if coverage had increased or decreased. Over that time period, the number of states that covered at least two treatment modalities increased from 2009 to 2021, and the number of states that did not cover any of the treatment modalities decreased from 2009 to 2021. However, we found a slight decrease in the total number of states that covered three treatment modalities from 2017 to 2021. Most surprisingly there was a reduction between 2017 and 2021 of coverage for pharmacotherapy; nine states dropped coverage.
In addition and for the first time, we attempted to collect utilization data from the states. Although utilization data were only received from 8 states, we found an underutilization of obesity benefits by plan enrollees when compared to each state’s rate of obesity. For example, the Texas Employee Retirement System, one of the state agencies that provided a complete data set for analysis, only 39 patients received bariatric surgery and only 5 prescription drug claims were filed. Additional research is needed to understand the scope of the underutilization of benefits when they are available, but we think that our findings emphasize the need to publicize these benefits to providers and patients, and to increase the demand for comprehensive obesity treatment services.
Despite the lack of progress in providing comprehensive obesity benefits, we acknowledge that there has been a concerted effort over the last two years to reverse this trend. Several advocates within states have been working behind the scenes to convince policymakers and administration to add coverage for all obesity treatments. For example, SEHPs in Georgia, Florida, and Arkansas have plans to add or expand coverage for pharmacotherapy in 2023.
To improve the treatment and management of obesity, coverage must be expanded. To do this, the STOP Obesity Alliance has made the following recommendations:
-
identify model obesity treatment coverage plans, and when coverage is available, assess the utilization of benefits;
-
encourage patients to demand coverage from their health plans and employers;
-
continue to advocate for expanded coverage from state employee health plans at the state capitols; and
-
increase studies of the return on investment to health plans and employers from covering all obesity treatment modalities.