ObesityWeek, the largest obesity conference in the world, took place this month. What were the takeaways? Most prominently, it is time for us to tackle childhood obesity, specifically severe childhood obesity.
We know that the rates of childhood and adolescent obesity have risen steadily over the past few decades, putting younger people at risk of obesity-related diseases typically seen in adults, such as type 2 diabetes. In response to these concerns, several sessions at ObesityWeek focused on the need for better treatments for children and adolescents, while addressing concerns that many have about putting children through the physical and psychological stress of obesity treatment.
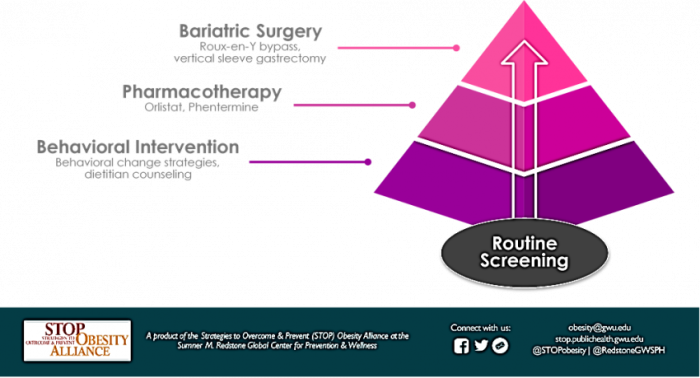
A new clinical update on the treatment of adolescent obesity, published in JAMA, recommends that adolescents have access to many of the same options as adults, ranging from behavioral interventions to surgery and including pharmacotherapy, depending on the patient’s BMI, preferences, and medical history.
In addition, new evidence supporting the safety and effectiveness of bariatric surgery in adolescents with severe obesity prompted the AAP to provide recommendations for bariatric surgery. The new recommendations urge pediatricians to assess their patients for severe obesity and refer them to surgical programs when appropriate. These new recommendations also address the barriers that stand in the way of those seeking bariatric surgery. One study found that over half of adolescents seeking surgical treatment for obesity were initially denied by insurance providers, most commonly because they were under the age of eighteen.
Unfortunately, the issue of reluctant insurers is not limited to bariatric surgery, and many evidence-based treatments are inaccessible to pediatric patients for financial reasons. Regarding pharmacotherapy, a lack of clinical trials is the most significant barrier that patients and physicians face. Only phentermine and orlistat have FDA approval for obesity treatment in adolescents.
Parents and the public have expressed worries that behavioral interventions, pharmacotherapy, and surgery could put children at risk of complications, including the development of eating disorders. However, research has shown that professionally administered weight loss programs pose minimal risk to children and adolescents. In fact, one study found that professional obesity treatment was actually correlated with a decrease in eating disorder symptoms. Parents considering talking to their child about their weight can consult our guide, Weigh In: Talking to Your Children About Weight and Health for suggestions.
It’s important to remember that for many children and adolescents with severe obesity, the benefits of treatment far outweigh the possible risks. It is imperative that children and adolescents have access to well-researched, evidence-based treatments for severe obesity. Researching the safety and efficacy of anti-obesity drugs for adolescents and advocating for insurance coverage for pharmacotherapy and surgery needs to be a priority. The focus that this year’s ObesityWeek sessions put on these ever-growing needs should serve as a call to action for the coming year, compelling researchers, advocates, and policymakers to redouble our efforts to facilitate the treatment of severe childhood obesity.