It is likely that the proportion of cancer cases and deathsattributable to obesity will continue to rise in the U.S. and globally over the next decade. Evidence-based interventions to promote healthy weight should be incorporated into comprehensive cancer control strategies for those with and without a history of cancer. Effective prevention of obesity-associated cancers will require a better understanding of the essential components for effective weight management, nutrition, and physical activity interventions, and guidance on how these interventions can be tailored to meet the needs of diverse populations.
Recent studies have provided ample evidence to link weight gain, overweight, and obesity with an increased risk for at least 11 types of cancer. An analysis of U.S. Cancer Statistics indicated that incidence of obesity-related cancers (excluding colorectal) increased significantly among adults 20-74 years of age during 2005-2014. Researchers from the American Cancer Societyestimated that excess body weight accounted for 7.8% of incident cancer cases (10.9% in women, 4.8% in men) and 6.5% of cancer-related deaths (7.4% in women; 5.7% in men) in 2014.
Figure 1 shows the estimated proportion of cases attributable to overweight and obesity by cancer type. Last year we developed an infographicillustrating that—along with increased risk for other chronic conditions—adults who gained 44 pounds or more between 18 and 55 years of age were 50-70% more likely than those who maintained the same weight to be diagnosed with an obesity-related cancer.
The absence of excess body fat lowers the risk of most cancers, so primary prevention of excess weight gain continues to be a critical target. Among persons who already have obesity, emerging datasuggest that weight loss may help prevent cancer. A handful of observational cohort studies and randomized control trials found that cancer incidence and levels of circulating cancer biomarkersdropped substantially following intentional weight loss through dietary interventions and bariatric surgery. However, additional research is needed to confirm these relationships.
Healthy weight management and physical activity also appear to be important for reducing morbidity and mortality risk among cancer survivors. In a 5-year study of more than 2,000 women with a history of breast cancer, researchers observed that a 3.7% lower average body weight was associated with a 24% lower cancer recurrence among the group randomized to a low-fat, reduced calorie diet (vs. standard diet).
A similar study assessing the effects of a low-fat, isocaloric dietary intervention found no difference in body weight or breast cancer recurrence, suggesting that weight loss is a key component of reducing recurrence risk among breast cancer survivors. Additional trials are needed to evaluate the impact of weight management interventions on quality of life, treatment tolerance, and long-term remission among survivors of other cancer types.
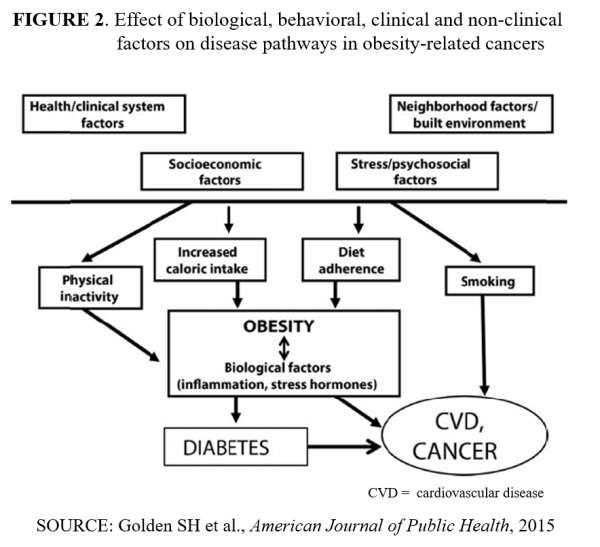
Like obesity, obesity-related cancers are not inevitable. Figure 2 suggests several places to intervene on biological, behavioral, clinical, and nonclinical factors that affect the development of cancer. There are numerous challenges in delivering weight management interventions across the cancer care continuum, including issues with reimbursement, infrastructure, program capacity, referral networks, clinician education, standards of care, and patient adherence. Still, the preponderance of evidence suggests that continued efforts to overcome these challenges will likely pay dividends in improving population health.