Download: Fast Facts - Mental Health and Obesity (PDF)
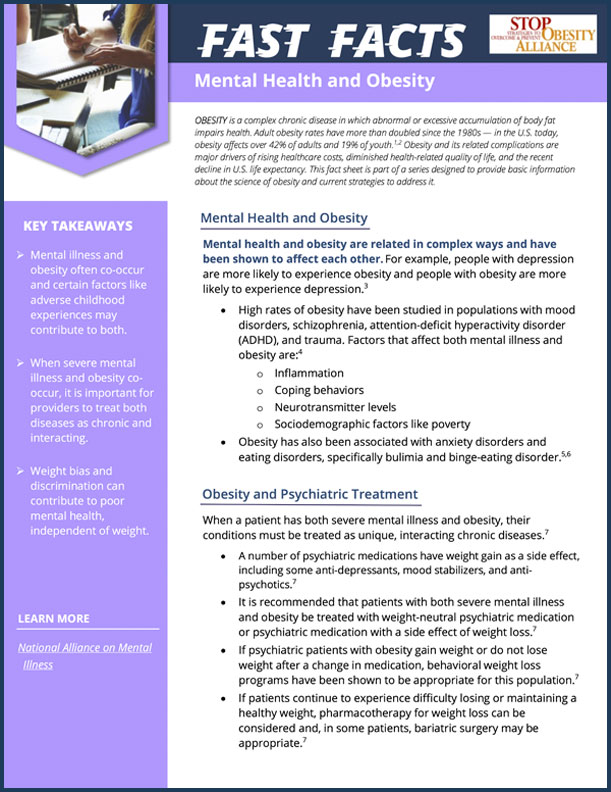
OBESITY is a complex chronic disease in which abnormal or excessive accumulation of body fat impairs health. Adult obesity rates have more than doubled since the 1980s — in the U.S. today, obesity affects over 42% of adults and 18% of youth.1,2 Obesity and its related complications are major drivers of rising healthcare costs, diminished health-related quality of life, and the recent decline in U.S. life expectancy. This fact sheet is part of a series designed to provide basic information about the science of obesity and current strategies to address it.
Key Takeaways
-
Mental Illness and obesity often co-occur and certain factors like adverse childhood experiences may contribute to both.
-
When severe mental illness and obesity co-occur, it is important for providers to treat both diseases as chronic and interacting.
-
Weight bias and discrimination can contribute to poor mental health, independent of weight.
Learn More:
Mental Health and Obesity
Mental health and obesity are related in complex ways and have been shown to affect each other. For example, people with depression are more likely to experience obesity and people with obesity are more likely to experience depression.3
- High rates of obesity have been studied in populations with mood disorders, schizophrenia, attention-deficit hyperactivity disorder (ADHD), and trauma. Factors that affect both mental illness and obesity are:4
- Inflammation
- Coping behaviors
- Neurotransmitter levels
- Sociodemographic factors like poverty
- Obesity has also been associated with anxiety disorders and eating disorders, specifically bulimia and binge-eating disorder.5,6
Obesity and Psychiatric Treatment
When a patient has both severe mental illness and obesity, their conditions must be treated as unique, interacting chronic diseases.7
- A number of psychiatric medications have weight gain as a side effect, including some anti-depressants, mood stabilizers, and anti-psychotics.7
- It is recommended that patients with both severe mental illness and obesity be treated with weight-neutral psychiatric medication or psychiatric medication with a side effect of weight loss.7
- If psychiatric patients with obesity gain weight or do not lose weight after a change in medication, behavioral weight loss programs have been shown to be appropriate for this population.7
- If patients continue to experience difficulty losing or maintaining a healthy weight, pharmacotherapy for weight loss can be considered and, in some patients, bariatric surgery may be appropriate.7
Weight Bias and Mental Health
In addition to the links between obesity and mental illness, experiences of weight-based discrimination have also been found to be associated with poor mental health. Research shows that weight bias is related to mental health independently; the relationship is not mediated by obesity.8
Adverse Childhood Experiences
Obesity and mental health are affected by many of the same contributing factors. One of these is adverse childhood experiences (ACEs).
- The odds of adolescents having overweight, obesity, or severe obesity increase if they have experienced adverse childhood experiences such as abuse, domestic violence, or parental incarceration.9
- Young adults who experience adverse childhood experiences have also been found to experience higher prevalences of depression, antisocial behavior, and drug use.10
- References
-
-
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief, no 360. Hyattsville, MD: National Center for Health Statistics. 2020
-
Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. NCHS Health E-Stats. 2020.
-
Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, Obesity, and Depression: A Systematic Review and Meta-analysis of Longitudinal Studies. Arch Gen Psychiatry. 2010;67(3):220-229. doi: 10.1001/archgenpsychiatry.2010.2.
-
Taylor VH, McIntyre RS, Remington G, Levitan RD, Stonehocker B, Sharma AM. Beyond Pharmacotherapy: Understanding the Links between Obesity and Chronic Mental Illness. The Canadian Journal of Psychiatry. 2012;57(1):5-12. doi:10.1177/070674371205700103
-
Bodenlos JS, Lemon SC, Schneider KL, August MA, Pagoto SL. Associations of mood and anxiety disorders with obesity: Comparisons by ethnicity. J Psychosom Res. 2011;71(5):319-324. doi: https://doi.org/10.1016/j.jpsychores.2011.03.004.
-
da Luz FQ, Hay P, Touyz S, Sainsbury A. Obesity with Comorbid Eating Disorders: Associated Health Risks and Treatment Approaches. Nutrients. 2018;10(7):829. Published 2018 Jun 27. doi:10.3390/nu10070829
-
McElroy SL. Obesity in Patients with Severe Mental Illness: Overview and Management. The Journal of clinical psychiatry. Supplement. 2009;70(3):12-21.
-
Hatzenbuehler ML, Keyes KM, Hasin DS. Associations Between Perceived Weight Discrimination and the Prevalence of Psychiatric Disorders in the General Population. Obesity. 2009;17(11):2033-2039. doi: https://doi.org/10.1038/oby.2009.131.
-
Davis L, Barnes AJ, Gross AC, Ryder JR, Shlafer RJ. Adverse Childhood Experiences and Weight Status among Adolescents. J Pediatr. 2019;204:71-76.e1. doi: 10.1016/j.jpeds.2018.08.071.
-
Schilling EA, Aseltine RH, Gore S. Adverse childhood experiences and mental health in young adults: a longitudinal survey. BMC Public Health. 2007;7(1):30. doi: 10.1186/1471-2458-7-30.
-
A product of the Strategies to Overcome & Prevent (STOP) Obesity Alliance at the Sumner M. Redstone Global Center for Prevention & Wellness.