With the extensive coverage of anti-obesity medications in the media, it is easy to forget or ignore the importance of promoting, researching, and advocating for intensive behavioral therapy (IBT) as a treatment for obesity. Many studies of behavioral interventions have shown success in helping patients control their weight while also reducing obesity-related comorbidities like type 2 diabetes. IBT has even been a core component of some trials for anti-obesity medications, and provides an important strategy for weight maintenance after weight loss with medications.
The Diabetes Prevention Program (DPP) emphasizes the importance of intensive lifestyle intervention programs. The DPP was a multicenter clinical intervention trial that aimed to prevent or delay the development of type 2 diabetes in those at risk for developing the disease. The study randomly assigned over 3,000 individuals with impaired glucose tolerance to either an intensive lifestyle intervention or to receive metformin or a placebo. The lifestyle intervention participants were given the goal of losing 7% or more of their body weight and reaching 150 minutes of physical activity per week. Each participant was assigned a case manager who assisted them through a 16-24 week core curriculum and maintained contact every two months for the remainder of the five year study.
The main results of the DPP found that the lifestyle intervention program reduced the risk of diabetes by 58%, or twice the risk reduction achieved with metformin. The lifestyle intervention program worked across genders, age and ethnic groups, and BMI subgroups. Participants lost an average of 14.3 lb at 6 months, maintained the loss at one year, and then gradually gained weight back for an average weight loss of 9.9 lb at the end of the study. Physical activity levels were also sustained at the end of the study. At a 10 year follow up, participants in the lifestyle program had regained some of the initially lost weight but did not return to the same beginning weight, ending in a net weight loss of about 4.5 pounds at the 10 year follow-up. This sustained weight loss is an important example of the role of intensive behavioral therapy as an significant component in comprehensive obesity care.
Weight changes for originally assigned treatment group since Diabetes Prevention Program (DPP) randomization for (A) all participants
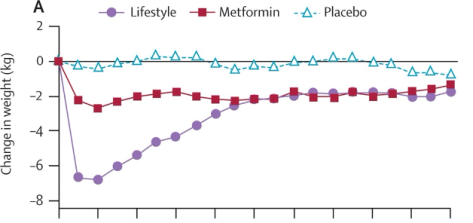
Years since program initiation
Source: Diabetes Prevention Program Research Group. (2009). 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. The Lancet, 374(9702), 1677-1686.
The SURMOUNT-3 trial reported the efficacy of the tirzepatide for weight loss after a successful intensive lifestyle intervention lead-in period. The study addresses the question of whether intensive lifestyle interventions can be an important screening tool to identify patients who might have the most success on anti-obesity medications. The double-blind study randomized adults with a BMI of >30 who lost greater > 5% of their body weight in a 12-week intensive lifestyle intervention program into a placebo or intervention group that received maximum tirzepatide doses for 72 weeks. All subjects were non-diabetic and had one obesity-related comorbidity. The mean loss of body weight was 21.1% for the tirzepatide group and 3.3% with placebo. Because a separate trial of tirzepatide without the lifestyle intervention lead-in was not conducted, it is unclear whether successful weight loss prior to drug therapy predicts greater weight loss after 72 weeks.
One of the main points of contention for payers as they struggle to decide whether to cover anti-obesity medications is the assumption that patients who start pharmacotherapy will need to remain on a drug for the rest of their lives to sustain weight loss. While more research needs to be done to understand the proper long-term care for patients taking anti-obesity medications, the positive effects of intensive behavioral therapy as a component of the maintenance phase of weight loss are promising.
The Treat and Reduce Obesity Act (TROA), which has been introduced in both the House and the Senate, aims to increase access to obesity care for patients in several ways, including expanding the number of healthcare providers who can be reimbursed by Medicare for intensive behavioral therapy. If passed, TROA would allow clinical psychologists, registered dietitians, and other nutrition professionals to bill for IBT outside of the primary care setting. Increasing access to behavioral intervention options is an essential part of obesity care.
While anti-obesity medications are already changing lives, clinicians need to understand and apply intensive behavioral interventions for treating obesity. The United States Preventive Services Task Force has proposed further research in this area with a focus on IBT delivered in primary care settings, which should be expanded on to include non-traditional providers of IBT.