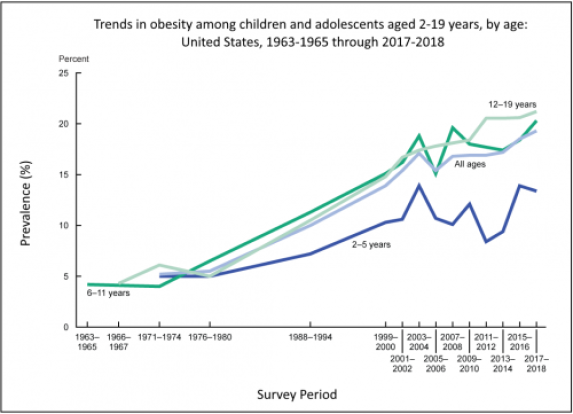
September is National Childhood Obesity Awareness Month. The obesity rate among U.S. youth has steadily increased since the 1990s. In 2017-2018, the prevalence of obesity for children and adolescents aged 2-19 years was 19.3%, or nearly one in five, and affected about 14.4 million children and adolescents. Obesity prevalence was higher among Hispanic and non-Hispanic Black children compared to non-Hispanic White and non-Hispanic Asian children. Obesity was also higher among households with lower education levels and lower incomes compared to the households in the highest education and highest income groups.
Source: CDC
Children with obesity have an increased risk of adverse physical and mental health consequences. Physical health risks include high blood pressure and high cholesterol, type 2 diabetes, asthma, and fatty liver disease. The increasing burden of type 2 diabetes among youth is of particular concern, because it has coincided with the increase in childhood obesity and reflects similar racial and ethnic disparities. Between 2002 and 2012, the incidence of type 2 diabetes among youth aged 19 and younger increased by 4.8% per year. The pathologic processes associated with diabetes progress more quickly in individuals with youth-onset type 2 diabetes compared to those with adult-onset diabetes, resulting in a greater risk of early diabetes-related complications. Children who have obesity are also five times more likely to have obesity in adulthood compared to their healthy-weight peers.
The mental health risks for children and adolescents with obesity include anxiety, depression, low self-esteem, lower self-reported quality of life, and social problems such as facing bullying and stigma. Early research shows the importance of taking psychosocial health into consideration when treating adolescents with obesity.
The COVID-19 pandemic has also seen an increase in the prevalence of childhood obesity; a study of pediatric patients aged 2 to 17 years found that obesity prevalence increased during the pandemic, with greater increases for Hispanic and non-Hispanic Black children compared to non-Hispanic White children. A cohort study in Southern California found that youths between 5 and 17 years old gained more weight during than before the pandemic, suggesting an increase in childhood obesity due to the pandemic. The pandemic has exacerbated the issue of childhood obesity through various mechanisms:
- Continuous stress on families and children; stress is a risk factor for the development of obesity.
- School closings, which exacerbate the risk of weight gain for children by eliminating access to school lunches and opportunities for physical activity. Research has demonstrated a significant decline in students’ physical activity levels, accompanied by increases in sedentary behavior, during school closures due to the pandemic. Because low-income communities already faced greater barriers to physical activity prior to the pandemic, the transition to virtual schooling only worsened these inequities.
- Breakdowns of the food supply chain and increased food insecurity, which in turn has increased reliance on ultra-processed foods. The consumption of ultra-processed foods was already increasing prior to the pandemic, across all levels of family income but especially among non-Hispanic Black and Mexican American youths. While further research is needed, recent studies have found that a higher intake of ultra-processed foods is associated with various adverse health outcomes in adults and with overweight and obesity in children.
As the issue of pediatric obesity continues to worsen, access to treatment for young people is a particular concern. Only three medications have been approved by the FDA for use in adolescents, and adolescents seeking surgical interventions have been frequently denied insurance coverage for the procedure. Other important barriers to treatment access for children and adolescents include the cost of and geographic distance to obesity intervention programs. These barriers must be addressed to expand equitable access to health care services for children.
The CDC has tips to help children maintain a healthy weight and the STOP Obesity Alliance has developed the Weigh In guide for parents on how to have conversations with their children about weight and health. For more information about childhood obesity, view our Obesity in Early Life Fast Fact sheet.