This month STOP is exploring a topic that is relatively new to us, the relationship obesity has with immune health. As research surrounding obesity continues to grow, we are increasingly learning about the impact that obesity has on health beyond weight.
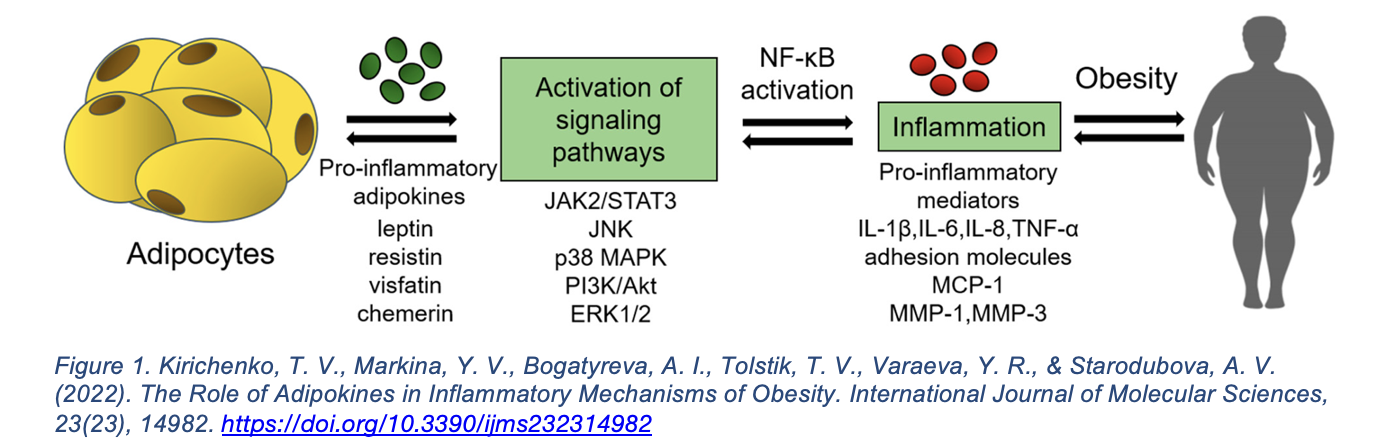
Traditionally obesity has been framed as excess body fat. However, it is also a state of chronic low-grade inflammation. This inflammation is caused by the release of inflammatory proteins by visceral adipocytes called adipokines. Over 600 adipokines have been identified; among those that contribute to inflammation include IL-6 and TNF-⍺. These signals attract immune cells such as monocytes into adipose tissue, where they differentiate into pro-inflammatory M1 macrophages (type of white blood cells), amplifying local and systemic inflammation. These adipokines induce insulin resistance, diabetes, and cardiovascular disease.
These inflammatory pathways disrupt the immune balance of patients with obesity, resulting in an increase in allergic diseases and metabolic disorders. Examples include higher rates of asthma, psoriasis, atopic dermatitis, and food allergies. The immune disruptions can complicate treatment for patients with obesity. Medications for these conditions often prove to be less effective, requiring higher doses and carrying greater risks due to the lack of research specific to patients with obesity.
The interplay between obesity and allergies, two seemingly unrelated topics, has immediate relevance for healthcare delivery, public health strategies, and insurance coverage. Further research into the connection between adiposity, inflammation, and immunity will promote a greater understanding of the implications of obesity beyond traditional understanding of the disease. The excessive release of adipokines can also increase the severity of infections like COVID-19. This connection emphasizes the importance of viewing obesity as not only a metabolic but also an inflammatory condition. Additional research will likely transform approaches to prevention, treatment, and policy and add to the complexity surrounding obesity. Attention to obesity’s role in inflammation is a key step toward building healthier and resilient patients and communities.