Last month, the Center for Biomedical System Design (CBSD) program at Tufts Medical Center's Institute for Clinical Research and Health Policy Studies in collaboration with healthcare providers, insurers, pharmaceutical companies, and patient advocates, published a comprehensive roadmap for transforming obesity disease management in the United States. The “Roadmap for Transforming Obesity Disease Management” presents a systems-level approach to obesity care, recognizing obesity as a chronic disease rather than a lifestyle choice. STOP Obesity Alliance’s Associate Director, Christine Gallagher, was a member of the work group that met over 18 months to develop the roadmap.
Obesity's complex challenges span from societal stigma and provider bias to fragmented care delivery and misaligned payment systems. System-level coordinated changes are needed across the entire healthcare ecosystem. The CBSD’s framework outlines three solution areas designed to improve US health systems readiness to treat obesity as a chronic disease. The three solution areas identified in the roadmap and detailed in the infographic below are:
- Patient Identification, Engagement & Diagnosis
- Shared Capability Building
- Integrated Care
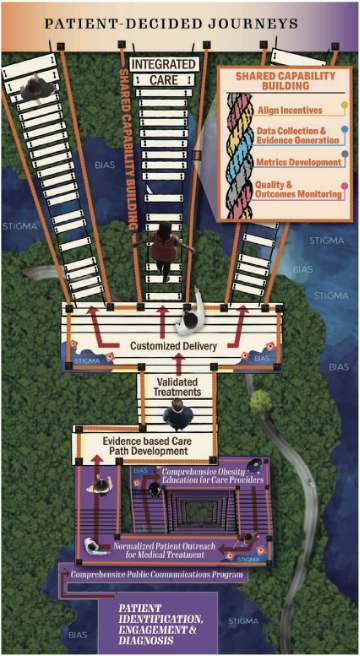
Patient Identification, Engagement and Diagnosis works to address stigma and bias through comprehensive communication plans, provider education, and normalized outreach processes. Represented by the purple staircase, finding appropriate care can be a challenging climb for patients who need providers and payers to proactively address obesity with medical treatment. Bias & stigma (represented by the blue swamp) must be waded through by both patients and providers to start engagement.
Shared Capability Building, represented in the figure via orange intertwined ropes and railings that support the other two solution areas, works to develop infrastructure that supports accountability, provides objective measures of progress, and enables knowledge sharing and continuous learning. Metrics development; data collection and evidence generation; aligned stakeholder incentives; and quality and outcomes monitoring form a rope handrail that provides structural support and handrails for all to grasp. These capabilities, if regularly updated, create continuous science-based improvement in an established learning environment.
Integrated Care works to deliver comprehensive treatment that is evidence-based and meets patients where they are. Represented by a tan platform and bridges in the infographic, this is where patients access multiple care pathways offering validated evidence-based treatment. Patients and providers work together through shared decision-making to select treatment. Treatments should be customized in their delivery to reflect the patient context and address capacity challenges (represented by missing boards in the bridge).
These three solution areas, with 36 specific action components, together make up the roadmap that can help lead us to the systemic changes needed in the current obesity disease care system. The full roadmap report is available at newdigs.tuftsmedicalcenter.org/obesity.


