Health care plans have taken vastly different approaches in determining what and how obesity treatment services are covered for their members. The diversity is in part due to the lack of guidance on how to operationalize evidence-based obesity treatments as health benefits. To complicate matters, incomplete information about what services are covered, for whom, and where, and how care should be delivered, is spread across various administrative plans, documents and policy sources in our fragmented care system.
As part of efforts to improve the treatment and management of obesity, the STOP Obesity Alliance has conducted research since 2009 that reviews how state insurance carriers cover obesity treatments and services. For example, in 2017, STOP conducted a state-by-state analysis of Medicaid and State Employee Health Plan coverage for obesity prevention and treatment.
State Medicaid programs have increased their focus on obesity treatment coverage. Some states have passed legislation to update obesity treatment coverage and other states are using regulatory pathways to modernize coverage policies. We expect to see more states to undertake reviews of their obesity treatment coverage.
To achieve a better understanding of what current Medicaid coverage looks like STOP partnered with the Obesity Action Coalition to contract with LEVERAGE, a solutions and consulting firm, to analyze the state Medicaid coverage data for plan year 2023. Both the Medicaid Fee for Service and top Medicaid Managed Care plans for each state were analyzed.
The Study
Our review of Medicaid coverage included the categories of comprehensive obesity care: nutrition counseling (NC), intensive behavioral therapy (IBT), obesity medications (OM), and metabolic and bariatric surgery (MBS). These data were extracted from Medicaid manuals, fee schedules, statutes, regulations, preferred drug lists, and managed care coverage when available. Only coverage for adults was considered.
A novel scoring approach was developed to analyze the level of obesity treatment coverage. We categorized treatment attributes as limitations and restrictions to describe the levels of coverage for obesity treatment. Each obesity treatment category was assigned a value according to the level of coverage provided. Each state was then assigned a total value based on the sum of the treatment categories assessed. The final values reflect whether overall obesity treatment in the state was covered, covered with limitations, covered with restrictions, or not covered.
Results
Our analysis is the first to investigate levels of coverage for obesity treatments. Even when coverage existed in the policy documents, we found limitations and restrictions that likely make treatments difficult to access, effectively making them not covered.
To determine whether a service was covered, plan documents were reviewed for language that addressed coverage, conditions of coverage, and exclusions from coverage. These data allowed us to describe specific limitations and restrictions that pose barriers to the utilization of these benefits. Details were available for stipulations such as medical necessity criteria for initiation and continuation of treatment, restrictions on site of care, conditions for care and coverage for revisions and corrections of surgical treatment. Many of the restrictions found did not align with clinical standards and guidelines.
The colors on the map reflect our results. Color scores were assigned to each state (including the District of Columbia) based on the number of treatment categories for which coverage was indicated and the limitations and restrictions to accessing obesity treatments.
Overall, obesity treatment coverage was “not covered” in fourteen (14) states and assigned the color red. An additional twenty-nine (29) states had “restrictive coverage” and were assigned the color orange. The final eight (8) states had “limited coverage” for obesity care and were assigned the color yellow. No state “covered” obesity care to achieve the color green.
Each obesity treatment category within each state was further explored to determine the level of coverage provided.
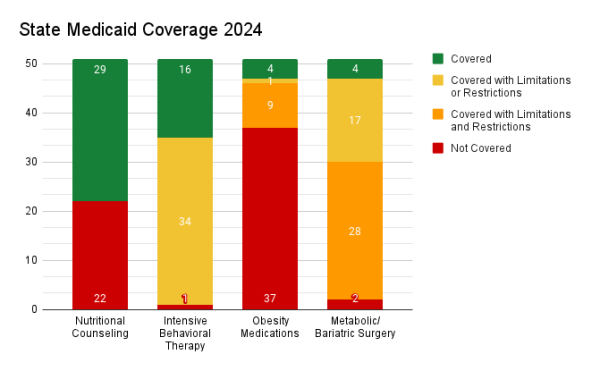
Twenty-two (22) states did not provide coverage for nutritional counseling. The remaining twenty-nine (29) states covered nutritional counseling.
One (1) state failed to provide any coverage for intensive behavioral therapy (IBT), thirty-four (34) states provided some coverage with limitations, and sixteen (16) states provided coverage for IBT.
No coverage for obesity medication was found in 32 states. Five states only offered coverage for over-the-counter medication (Orlistat/Xenical/Alli) for obesity; which we categorized as not covered. Nine states covered obesity medications but with limitations or restrictions. One state provided limited coverage for only one class of medications. Four states covered obesity medications. Of the four states that covered obesity medications, two of them cover medications in statute, but no medications were listed in the preferred drug list for that state’s Medicaid program.
Medicaid coverage for metabolic and bariatric surgery (MBS) was not covered in two states. Twenty-eight (28) states covered MBS with limitations and restrictions. One state covered MBS with limitations and sixteen covered MBS with restrictions. Four states provided full coverage for metabolic and bariatric surgery without any Medicaid limitations or restrictions.
In conclusion, we found that obesity treatments in state Medicaid programs had several levels of coverage, within and across treatment categories. Coverage for obesity treatments often came with limitations and/or restrictions that added complexity to accessing services and benefits. Across all evidence-based obesity treatments, no state provided coverage for comprehensive obesity care. All states applied various levels of exclusions, limitations, or restrictions for the coverage of obesity treatments.
Application
The good news is that some of the restrictions that we found could be easily corrected to improve the quality of obesity care, and not all of them would need to be done through statute. The other good news is that now that we know the state of care for obesity in the state Medicaid programs, we can arm our advocates with what they need to convince policymakers and administrations to increase access to obesity treatments in each state Medicaid program.